Abstract
Introduction: There is conflicting evidence regarding the association between poverty and survival in children with cancer. Most studies have relied on surrogate indicators of poverty, such as zip code-based median income for area of residence or on insurance status (Bona, PBC 2016; Kehm, Cancer 2019; Bona, JNCI 2021). We hypothesized that household poverty (measured at the individual level, using self-reported annual household income) during maintenance would be associated with a greater hazard of relapse among children with ALL.
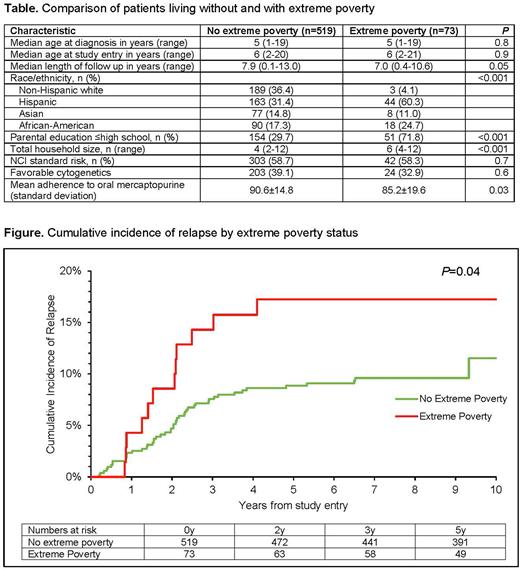
Methods: In this secondary analysis of COG-AALL03N1 (primary aim: adherence to oral mercaptopurine during maintenance), we examined the association between household poverty during maintenance and relapse risk in children with ALL. Eligibility for enrollment on AALL03N1 included (1) age <21y at ALL diagnosis; (2) receiving maintenance therapy in first remission. The current analysis was restricted to patients living in US who provided information on annual household income and the number of household members. We used national yearly median poverty thresholds provided by CDC; these take into account the annual household income and the size of family unit (i.e., number of adults and children <18y). For example, the annual income of a three-person household (two parents and one child [patient]) would need to be >$14,480 to be above the poverty threshold in the year 2002 (or >$21,831 in the year 2021). Among those below poverty threshold, we classified families with annual income under 120% federal threshold (median percent below poverty threshold for this cohort) as living in extreme poverty. Hazard of relapse from study enrollment during ALL maintenance therapy was estimated using proportional subdistribution hazard regression models, treating extreme poverty as the primary exposure and adjusting for age at study, sex, NCI risk group, blast cytogenetics, average 6MP and methotrexate dose intensity and time from start of maintenance to study entry.
Results: We summarize sociodemographic and disease characteristics of 592 eligible patients in the Table. Median household income of the cohort was $35,000/year (range $10,000->$150,000). Overall, 73 (12.3%) patients met criteria for extreme poverty. Families living in extreme poverty were more likely to self-report their race/ethnicity as Hispanic or African-American and report parental education as high school (HS) or lower. Of note, clinical factors did not differ by poverty level. In a logistic regression, non-white race/ethnicity (odds ratio [OR]=7.9, 95%CI=2.4-26.1, P=0.007; reference: non-Hispanic white) and low parental education (≤HS: OR=4.2, 95%CI=2.4-7.4, P=<0.001; reference: college degree or higher) were associated with greater odds of living in extreme poverty. Cumulative incidence of relapse at 3y (Figure) from study entry among patients living in extreme poverty was higher compared to those without extreme poverty (14.3% [95%CI, 7-24] vs 7.6% [95%CI, 5-10], P=0.04). Patients living in extreme poverty had a 1.97-fold higher hazard of relapse compared to those not living in extreme poverty after adjusting for above mentioned covariates (95%CI=1.03-3.76, P=0.04). The reasons for the association between individual level poverty and relapse risk are likely multifactorial and possibly include poor adherence to oral chemotherapy. We found that patients living in extreme poverty had lower adherence to 6MP compared to those not living in extreme poverty (85.2±19.6% vs 90.6±14.8%, P=0.03).
Conclusions: Extreme household poverty is associated with increased hazard of relapse in children receiving maintenance therapy for ALL compared to those living without extreme household poverty. Mechanisms investigating this association need to be explored in future studies.
Disclosures
Dickens:Tempus: Consultancy. Landier:Merck Sharp & Dohme: Other: Wendy Landier's institution has received vaccine supply and laboratory services for an unrelated clinical trial through the Investigator Initiated Studies Program of Merck Sharp & Dohme (MISP #40083).
Author notes
Asterisk with author names denotes non-ASH members.